DR. MIKE MORENO: Welcome back to Wellness Inc. I’m Dr. Mike Moreno taking a deep dive into all things wellness after over 25 years of practicing medicine. I’m fascinated with anything and everything that can help you feel better, live healthier and become the best you possible. I’ll be interviewing the most cutting-edge experts in the field of wellness and exploring new innovative technologies to help you live your best life. At the end of each episode, I’ll give you my weekly RX. My top tips for you to use right away. Remember to subscribe for free, rate and review my podcast on Apple Podcasts or wherever you listen.
We have an important show for you today, straight from the front lines of COVID 19. I know we’re all tired of hearing that phrase. It’s January 2021, the start of a new year and we’re still in the middle of this global pandemic, hopefully light at the end of the tunnel, but right now, we’re having and experiencing some serious surge in cases and we have just the right person. We’re so fortunate with us today to give us the latest information we need to take care of ourselves and the people we love.
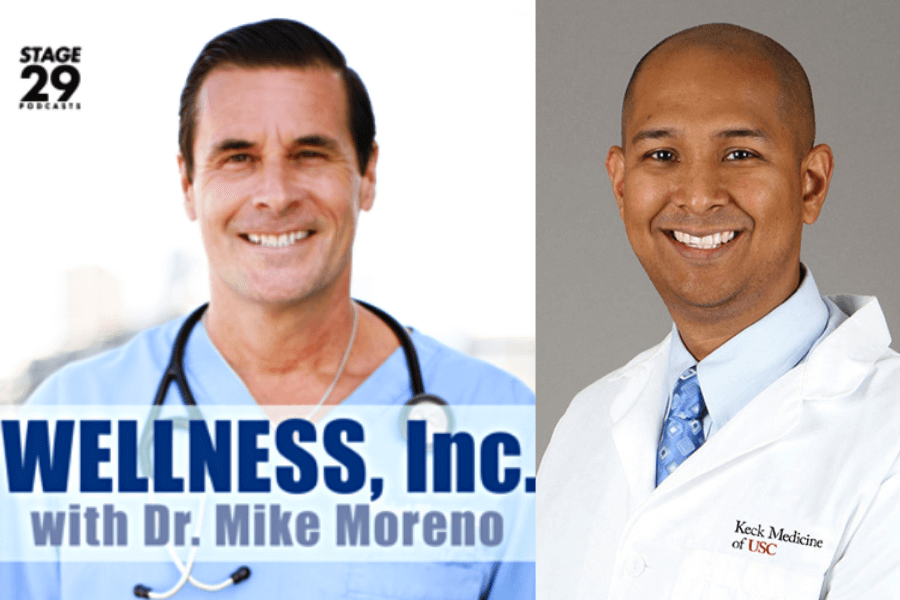
Dr. Raj Dasgupta is 4 times board certified, which let me tell you, is a lot of work my friend, In internal medicine, pulmonary critical care and sleep. We’re going to talk about all of this stuff. He has his own series of medical books called Beyond the Pearls. You may know him from being a regular on The Doctors television show for 7 seasons or from being co-host on Chasing the Cure with Ann Curry. He has his own podcast called The Dr. Raj Show, which you should check out if you haven’t already. His passion is teaching, and he is an associate professor at USC right now, working on the front lines in the area of pulmonary critical care, dealing directly with life and death situations every day. Welcome to the show, Dr. Raj Dasgupta.
DR. RAJ DASGUPTA: Oh, thank you, Mike, and I got to tell you, that was one of the best intros. I know how many times you practiced it, but I mean, it was I got to tell you, I’m jealous. I hope I can record that and replay it over and over again. Thank you so much for having me on your show. I really, truly appreciate it.
DR. MIKE MORENO: Thanks for being here and listen, I want to get right into this because, you know, I’ve been practicing medicine for 22-ish years. I have a lot of dear, dear friends in the ICU, both nurses, staffing and anybody and everybody. You know, we tend to think of nurses and doctors, but we don’t even think about sometimes the ancillary staff, people who clean these rooms, people who I mean, being in an ER in an ICU setting right now is a scary, scary thing. Tell us before we even get into that, why don’t a lot of our listeners are probably like, what exactly is pulmonary critical care? I think he could possibly get an idea, but why don’t you just spend a minute or two talking about what that is?
DR. RAJ DASGUPTA: You know, pulmonary is the lungs, and that’s my passion to help you breathe, so get that oxygen right into the bloodstream and get it to the tissues that need it, that’s going to be a pulmonologist. What diseases do I see? Well, let me throw out some common names. How about COPD? (Don’t smoke anyone). What about asthma and allergies? Now one of my passions is pulmonary fibrosis, which goes undiagnosed. But of course, when we talk about COVID 19, it affects every organ in the body, but the number 1 organ most commonly involved has to be the lungs, and that’s why I’m going to be involved with that. When I mention critical care, well, that’s where the sickest patients in the hospital are going to be in.
Right now, any time you turn on the news, what do we say? The issues are at capacity and that is the truth, and people in the issues are on these ventilators. I got to tell you, when we get to that part of the conversation, if you want me to start crying on your podcast, talk about people on the ventilators. That’s why many lung doctors do critical care because patients need that assistance to breathe. I would say now, more than any time in my life, I’m so proud I trained in that subspecialty because it is truly an honor and scary to help out in this pandemic right now.
DR. MIKE MORENO: I can’t imagine when you went into your particular in the ICU and working as an ICU doctor, which has to be the most stressful thing ever that you ever imagined you would see what you’re seeing now. I mean, what are you seeing right now when you put on that lab coat and you hang that stethoscope around your neck and walk into that ward? I cannot imagine what goes through your mind.
DR. RAJ DASGUPTA: Well, if you were to ask me this question in the beginning of the pandemic and right now, my response is always going to change. In the beginning of the pandemic, I was scared. This is the first time I’ve experienced, you know, a virus that we have very limited knowledge about that you hear is infecting everyone, it’s killing people and you’re just going to walk into that room. So, there was a lot of just anxiety right there. Then right now, if you were to ask me the question, I think the first word out of my mouth is going to be just, I’m humbled because during this whole year, every time you try to get ahead of the virus, we think we solve the rubik’s cube. We didn’t. Every time we thought we had a drug that was going to be the magic bullet, we don’t. It always makes me appreciate the science behind trying to get the right answer. And teamwork.
Mike, you brought it up earlier, is that it really isn’t just the doctor. I’ve never appreciated all the people around me that make me a better person. My nurses, the people who clean the room, the respiratory therapist, the pharmacist. When we talk about ICU’s at capacity, it’s not just the literal bed. It’s the people who are so fatigued that have to keep pushing. So yes, I’m honored. Yes, I’m privileged, and I will. I have to give a shout out to my amazing medical residents, my internal medicine residents and my pulmonary critical care fellows. All of those, they kick ass. They’re hardworking, and they definitely deserve some credit.
DR. MIKE MORENO: Got it. I’ll tell you right now, I can imagine if you’re an intern coming out of med school, right, you’re just bright eyed, bushy tailed, you’re now an intern. Talk about the worst timing ever. I can’t imagine. I think what fascinates me is, and you kind of commented on this when you go back and look at how we were managing patients in April vs how we’re managing them now, never before have we seen such an evolution in both disease presence and management and treatment in nine months. I mean, what are your thoughts on, you know, traditionally you’re like, Oh, two sets should be this. You can’t imagine letting a patient walk out on this, yet we’re watching guys walking around having perfect conversations stating in the 70s. Like, it must be like, weird to you, right?
DR. RAJ DASGUPTA: I’ve never seen someone in a room, on their cell phone and your oxygen saturation is going to be in the 80s and only now during this pandemic. But you know what? There are some things we are doing right. One of the big things was during the pandemic started, patients needed to go on that mechanical ventilator. I could tell you that that was one of the things I wish we could take back a little bit because of the fact that once you’re on that mechanical ventilator, it, it’s just scary. You’re going to be isolated from your family, you’re going to be on that ventilator for weeks, if not even months. We need to use medications that will keep you sedate and calm, and it’s horrible.
Now, as we’ve learned more, we have better techniques to help prevent throwing people on the ventilator right away. It’s probably the biggest claim to fame is putting patients on their stomach. We call that the prone position, and this is something you could do at home, something you tell your family and friends to do if they unfortunately get COVID. We knew about this putting them on their stomach prone position from other diseases in the past. But it works so well for our COVID patients. We don’t know why, but we’ve learned newer techniques to help prevent putting patients on the ventilator. let me just say one more thing about medications that out of all the medications we’ve been trying throughout this pandemic, who knew that the best medication will be an old medication we’ve been using for a long time, which are steroids. We had a study that showed it improved survival in our sick patients.
So, I’m going to say that we’re on the right track doing some good things.
DR. MIKE MORENO: It’s interesting because instinctively, I remember in April, you kind of talked about this a little bit for many viruses have a predilection towards different body parts, organ systems, whatever we may see, I think it’s fair to assume that a good majority of them have a pulmonary impact. The respiratory system, it’s an inflammatory process. We talk about inflammation throughout the body for multiple disease states. I find it interesting that this bug comes in basically creates chaos. It’s like inviting 10 five-year-old’s into your house and letting them run around and destroy everything and then you have to put it back together. So, tell us what it was like to kind of been taught these things all your life and then all of a sudden you’re like, wait a minute, we’re supposed to do this, and we’re supposed to do this, and now you’re changing what you’re doing. Is it kind of an odd thing to sort of you’re going back and almost relearning your profession in a sense.
DR. RAJ DASGUPTA: Oh, yes. That’s the part of being a doctor, I’m sure you’re the same way, Dr. Mike. It’s lifelong learning. It’s annoying to admit that when you don’t know something and you know, even when after this pandemic is starting to go in a good direction. Trust me, there’s going to be COVID clinics. There are going to be what we call the long haulers. I’m already getting some of these questions about, Hey, I have this brain fog that doesn’t go away. I had this fatigue that doesn’t live leave me. I have some muscle aches. What are my lungs looking like now? They told me I had COVID pneumonia, are my lungs ok?
So, this is a whole different podcast in conversation talking about what’s going to happen down the line and we need to learn more about it. But you know, in the hospital right now, I think the biggest thing that changed the game in our favor was that we realize there’s no organ that’s spared with COVID. It affects the heart. It can give you heart failure. It can cause arrhythmias. It can cause clotting in the body, in the arteries, in the veins. You know what’s scary? This clotting could happen after you leave the hospital. So things that I normally would not order normally would not think about. You’ve got to think about it right now.
So, you know what? I think that this is going to be something that really change the way we approach medicine, the way we approach being in the hospital. I think for an educational standpoint, it’s a good thing, not a bad thing.
DR. MIKE MORENO: I think one of the most interesting things to me, I was talking to a buddy of mine just last night and I hadn’t talked to him for a while and really thick guy. We’re both in our 50s and, you know, I like to think, you know, I exercise every day and I take care of myself as does he and I told him because he and his whole family got it, which we’re going to go to that in a second, but it’s odd to me that I had a family, 3 individuals in their 60s, all relatively healthy individuals. One person unfortunately passed away. One person got extremely ill for several months and one person never got it.
Now, we don’t know whether they were false negatives or, you know, that’s a whole other, you know, discussion, but it’s such a bizarre, bizarre disease to me and we can’t make sense of it. And anybody who has all the answers run away from that person because they don’t know what they’re talking about. If they think they have all the answers. What do you think about that? There are so many things out social media, whatever. Everybody’s got an opinion. What are your thoughts on that?
DR. RAJ DASGUPTA: Dr. Mike, I got to say you don’t look like you’re in your 50s. Not to build up your ego or anything. The truth is the media can be helpful, but it can be hurtful sometimes, too. I think it has been confusing for many individuals. The classic example is now Dr. Mike, some of you heard this. Are they asymptomatic or pre-symptomatic? This terminology is just going to be very confusing. I don’t even know what the difference is.
And then when you talk about how many days you need to be in quarantine, well, it’s 14, but then it could be 10 if you do this, if you do that and this is not for people like me and you, Dr. Mike, we’re talking about the general public and it can be very, very confusing. Testing now, you try to teach testing to the general public. Is it an antigen? Is it an antibody? Is it the PCR? I mean, people are confused.
The most common example I could think of right now about the media was when we’re talking about vaccines and you know, I am on the bandwagon of getting everyone vaccinated, I want herd immunity in the right way, but when those two individuals in the U.K. got anaphylaxis, that was the news. You know what I mean for any time you open the station, and it scared a lot of individuals. I think that the media needs to be careful and select and how they choose things. But beyond just the media, you know, even the CDC, the World Health Organization, it just seems that we weren’t on the same page when it comes to this virus and this pandemic.
So I think in the future, hopefully we can be better communicators. We have a simple message. I think Dr. Mike, one of the biggest skills in trying to be a good doctor is not just how much knowledge you have but communicating just to the general public. It’s actually tougher than you think.
DR. MIKE MORENO: Yeah, and I feel for people in the media. I think we have a responsibility to deliver adequate, accurate information, but I oftentimes feel like it’s done in a way that is meant to get ratings and not to really create a sense of awareness vs panic. Those are two distinctly different words. Awareness and panic are two, and I’ve seen examples of both, and I just think that’s not very nice. I’m a doctor and it frustrates and panics me a bit. Imagine what the general public must think when you’re throwing this stuff out there, there’s really an element of irresponsibility there. I think we need to be aware. We need to be informed, but I don’t think panic to create interest is the way to go about it. You touched on that a hundred percent.
DR. RAJ DASGUPTA: Let me let me say this, my wife, she’s a rheumatologist and I feel bad for her because when this pandemic first started, everyone and the family dog was on hydroxychloroquine and my wife, a rheumatologist, deals with people with lupus and people with other diseases. There was a shortage out there, and then for a short period of time, there was a medication called colchicine and use it for gout, and there was a little data about that. Then all of a sudden, my wife’s patients with gout couldn’t get their colchicine. So, media people doctors do not realize is that when you hype certain medications up certain supplements up, there is a secondary effect that happens that people don’t realize.
DR. MIKE MORENO: Yeah, interesting, my sister has rheumatoid arthritis, and has dealt with it for years and on steroids and the whole nine yards, she said they’re kind of telling me, I may not be able to get a lot of my hydroxychloroquine. I said, relax, they’re just rationing because of what’s been stored up in the media. But you’ll be fine. But it’s it really is. It’s outrageous. I mean, even my buddy yesterday I was talking to him and he was like asking me, he’s like, What about this? I said, Listen, those were those were literally minutes in time where someone thought, Hey, maybe this is something and then someone took that and ran out and screamed it to the world, and It caused a lot of panic. So, all right, so I have to ask you this. I’m talking to my buddy last night and he’s telling me that he and his wife and his kids, the whole family got COVID. How does that resonate with you? And does that ring a bell?
DR. RAJ DASGUPTA: Yeah. So, Dr. Mike, around end of July, beginning of August, my my wife and I have 3 kids. I have a 9-month year old. Her name is Sadie. I have a 5-year-old named Aiden, and he has autism and I have Nina, my 7-year-old, and we all got COVID. The story was, is that we really didn’t know if it was my wife. She is a physician or was it me? Because you know the saying you go to the barbershop enough, eventually you’ll get a haircut, and my wife brought home the COVID haircut. The way that the symptoms presented was actually in my 9 month old, it really was nothing. She had a little runny nose, and it could be a plethora of common cold viruses, and we did not think anything about it, but then around July, my daughter Nina, a 7-year-old, was going to go to a camp and my wife and I said she just wasn’t looking good, just kind of achy and we do want to put any family at risk. So, we get tested, and when my wife brought my daughter to get tested, they wanted to put that little nasal swab up her nose and she was like, “hell no”. She didn’t say hell, so, when she was crying, my wife who was there, said, I’ll get tested too. Little did we know that was $250 for that test, but she got tested and here’s the sad part at the time, it took 5 days to get the results. So, 5 days later, my daughter and my wife were positive. My wife was running at the time with the mask, but it’s just that feeling of almost tunnel vision. She was scared. She came home. We had to tell my daughter because we had to say, Hey, no camp for you this year. There was tears and crying. I told my work I got tested. And of course, because I’m lucky, I’m part of a university, I got tested in two seconds. Results come right back. I’m positive and there you go.
At that time, we didn’t know much about the virus where things were going, but you know, someone loves us. We all did well. We all had very, very, very mild symptoms. Before I got my vaccine, they tested my antibody. So, if I had the antibody, they weren’t going to give me the vaccine appropriately and I don’t have immunity. So I know there were recent studies outside, showing, well, how long does the immunity last? I’m going to tell everyone; I know the magic number everyone wants to focus on is 6 months, but don’t hyper focus on that, but that immunity doesn’t last forever, and I end up getting my vaccine about 3 weeks ago.
DR. MIKE MORENO: Yeah, the truth is, never in medicine has it been more appropriate to say, we don’t know because quite honestly, we really don’t. Let me ask you a question. I’m curious what you think because I was saying this like I know everything like months ago, I was telling my friends and colleagues they were like, shut up. I said, this is going to be the best flu season we’ve ever had in our lives, not because of the vaccine, but because everybody is doing what we are supposed to do when we’re sick. You know how many times, everybody’s listening out there?
Dr. Raj, I’m sure you can agree how many times if we’ve been out with our friends or family and someone’s kind of sniffling or congested and you’re like, Hey, you’re not feeling good. Yeah, I just got a little cold. It isn’t happening now. Anybody who likes sneezes in public, you look at them and like, you’re like running for the hills. So, I think, do you feel like the flu season is almost nonexistent this year? I hate to use that word, but because of the social measures and all of the hygienic measures, what do you think?
DR. RAJ DASGUPTA: Yeah, when I was getting doing some interviews for the news, I would say in like like late September, early October, when you should start thinking about the flu vaccine, what was the buzz word, the “twindemics”? It sounded like some kind of Walking Dead movie title, and I would go on the news and talk about the “twindemics”, and it is scary if it did happen, but you know you’re 100% correct. I think that we were very lucky for those who don’t know how we create our flu vaccine is that we take the data and information from the opposite side of the world when they have their flu season before we do. They’ve been lucky. They had very mild strains. They did not have scary things like H1N1 this year. Thank god, and we have a milder flu season.
In general, you hit the nail on the head, Dr. Mike, the things we’re doing now is the same things you do for the common cold, the same things you do for the flu and it’s good. And to really show how what a curveball you know, COVID 19 is, is that we thought we could get ahead of this during the summertime. We thought all the heat here in wonderful California would kill all the virus, but it really did not. Then all of a sudden, why is it getting worse now? You can’t pick the worst time to flare up for COVID 19. It’s winter. People are together. People are caroling out loud without a mask, and then it’s one vacation after another. You know, I’m always not the one to point fingers because everyone has their own story of why they travel or didn’t travel. I don’t want to be that guy, but it’s been poor timing, and that’s why we’re stuck in this horrible surge right now, especially here in my hometown in Los Angeles. We’re getting kicked pretty hard.
DR. MIKE MORENO: Well, I got to tell you what’s kicked me pretty hard, and I’ve always sort of struggled with it a bit is sleeping. As a primary care guy, oftentimes patients come in and you kind of have to go through that first layer of the onion, as I call it, which is they don’t come in saying, Doc, I’m stressed. They come in saying, you know, Doc, I have this rash or Doc, I feel itchy, or I’ve had more headaches, or my stomach has been upset.
Then as you peel back the layer of the onion and your eyes start watering, you recognize it’s stress, it’s anxiety, it’s lack of sleep. I’m praying that you agree to come back and talk to us just on sleep. I will promise my listeners that you will without even getting your approval because I need to hear. I’m just being, you know, selfish. But if you could tell me for a second what? Because again, I know you’re boarded on four levels. One being sleep. What have you seen in terms of COVID and sleeping and the impact? What is what is that like?
DR. RAJ DASGUPTA: Sure. I had an interview recently about this, and it was one of my favorite interviews with one my patients. They just been dreaming more and we talk about these dreams. These are going to be vivid dreams. These are going to be dreams that they actually remember. Sometimes it could actually be nightmares. So when we talk about why, why is this happening? Why are people dreaming more during a pandemic?
A couple of reasons. They did a study that showed during the pandemic we have right now, total sleep time has increased in the United States by 20%. So the more time you have the sleep, the more time you have the dream. Also, that all my patients, the majority of my patients, they’re going to bed even later and they’re waking up way late in the morning. They are all a bunch of night owls. Now everyone is going to be a night owl. What happens when someone tells me they’re having more dreams based upon our sleep schedule, we get most of our REM like dreams in the morning. REM dreams are vivid, and those are the ones that are like nightmares.
So, this is the reason why we’re having nightmares, why we’re having more dreams. And it’s not surprising because they did studies when we had that horrible tragedy at the World Trade Center. During that period of time, people were having more nightmares and everything.
So what am I seeing? I’m seeing more people who are having insomnia. It is just multifactorial. This insomnia could be because of the fact that they are stressed. There is anxiety, there is depression, and even the medications we use for depression can cause insomnia. We are having people, whether it is a patient or whether it is going to be a health care provider like you and me, we are getting anxiety and PTSD, and that is a huge thing I’m thinking about right now.
And just on another note, we’ve been joking about weight throughout this pandemic. I think one of the phrases that puts a smile on my face is that a lot of people gain the COVID 19. You know what I mean? The 19 pounds. One of the sleep disorders that has affected 15 to 20 million Americans is called obstructive sleep apnea. With the weight gain we’re having now. I just wonder where that is going to pan out when you start getting a chance to diagnose and dive into it again but sleep definitely took a big shot when we talk about this pandemic.
DR. MIKE MORENO: Yeah, I talk to people all the time and, initially when they were talking about who was the most vulnerable and they were saying the elderly and comorbid conditions and all of these things, I honestly and I may be wrong. Who am I? What do I know? I feel that first of all, the next three to five to seven to 10 years, we are going to learn so much about this disease. It’s going to be fascinating. There are going to be volumes and volumes and volumes of things, and I’m sure your name is going to be on some big volume of sleep and COVID. I think we are going to look back and we are going to find out that it wasn’t necessarily the elderly, it wasn’t necessarily the comorbid, although of course they are high risk. I’m not saying that I think it is going to be obesity and poor level of fitness. This, to me, is a disease, not entirely, you commented on this, it is a respiratory illness. Its impact, its inflammatory impact on the on the respiratory system. We know with sleep apnea, we know with people who are obese, they have poor ventilator capabilities, and when that happens, you are at a risk.
And I really feel like when we look back and you know, it’s already being talked about, the United States has the most cases, the most deaths, the most issues with this, that and the other. You know, when they talk about it all the time, and let’s not just leave any stone unturned here. We have the biggest issues with obesity. We have the biggest issues with it goes on and on and on. I think there is a direct correlation there, and I think we’re going to look back and learn that, hey, the best thing you could have done for yourself was not getting that COVID-19 was to lose COVID-19. Get yourself in a healthier place, both from mentally, physically fitness weight, you name it. What do you think about that? Because I’m going to be dragging you down with me if I go down.
DR. RAJ DASGUPTA: So, number one, I have this conversation with my wife, she’s a rheumatologist and people who are obese, they have that extra adipose tissue. There were studies that show they have higher levels of inflammatory markers. It’s not a secret. That’s why obesity plays a role when we talk about pain in all these other diseases, aside from COVID, but you are right. When I talk to you right now and we talk about COVID, I just close my eyes and think about my patients I saw in the ICU yesterday. And you’re right, they are overweight. They are obese, and these are things that if there’s anything you could work on to help prevent get disease, this is something that easier said than done, but yes, work on that diet, work on that exercise. And it definitely does make a difference when we talk about that.
That’s where I think that sleep and being overweight, there is a correlation there. There’s a correlation where if you have insomnia at night, I’m sure just by instinct, when you’re up late, you’re not grabbing Avon water and celery. I’m not sure what you’re up with your cool ranch Doritos, and choco-tacos.
On top of that, from a medical standpoint, there are many hormones that are in play. Let me get just a little dorky that in people who have insomnia, the 2 weight hormones that jump to mind are called Leptin and Ghrelin. Leptin stands with the letter L. It stands for lose weight, and when you’re sleeping, you get more secretion of leptin to help lose that weight.
When you have insomnia, when you have multiple awakenings and arousals, you get the G. The G stands for Ghrelin, which is gain weight. So, all of these hormones, there is some science behind this, and I agree clinically, the risk factors that we’ve already determined, obesity is one of the highest ones. I agree with you, Dr. Mike.
DR. MIKE MORENO: I can’t thank you enough. We’ve got to bring you back to talk about sleep because my god I am working on a book now that will hopefully be coming out at the end of the year. I did a whole chapter on sleep and I preach sleep hygiene to my patients. That’s a whole other volume of conversation. Listen, I cannot thank you enough. Honestly, this is from my heart. I thank you for what you’re doing because I have friends, I have colleagues, I have people who are in that hospital and I want this thanks to go out to anybody who’s out there, who’s dealing with this on the front line.
Quite honestly, anybody in the world, anybody who happens to be listening to this, this is just a bad thing and it is unfortunate, and it pains me, and it gives me this sort of swelling in my throat when I think about it. But we’re going to get through this and with the help of Dr. Raj and his staff and all of the people out there, from nurses to doctors to staff to people in that hospital when they walk in, these guys are doing a fantastic great deed.
I thank everyone and Dr. Raj, where do we find you because people are going to be knocking down your door?
DR. RAJ DASGUPTA: Yes. Well, before I tell you where I am, Dr. Mike, thank you for letting me be on the show and my compliment to you is you’re a cool dude. I like talking to you and I truly mean that. It’s great to have a break from the ICU to come do this. It really is a nice change of pace because it is stressful, and it’s sometimes it’s nice to kind of just relax and have somebody who understands what we’re going through. If you want to find me two things I would say check out my podcast and if one day Dr. Mike is nice enough, maybe he could appear on my podcast one day.
DR MIKE MORENO: I’m in!
DR. RAJ DASGUPTA: And yeah, I’m on Instagram. You could just put Dr. Raj, find my handles, Twitter, all the things that are out there. And if you are a medical student or in the medical field, I am super, super proud of my book series. It is called “Beyond the Pearls” because I really want everyone in life to go beyond…don’t settle, go beyond. And this is a book of cases throughout medicine or surgery, psychiatry, sleep. So, check it out, ok?
DR. MIKE MORENO: Thank you. Well, there we have it. Dr. Raj Dasgupta, I could talk to this guy forever and in fact, now we all have his handle, we can get a hold of him. I mean, we’ve got to bring this guy back on and talk about sleep. Thank you. Thanks so much. Ok, now it’s time for our week RX!
I was trying to frantically think about all the things I wanted to talk about, but I keep this simple we didn’t even get to the sleep thing which is driving me nuts, but I got to tell you the first tip I want people to do is do what you’re supposed to do. We all know what that is. You know, my mom and dad taught me when I was a little kid. Wash your hands. You know, don’t touch your face. Exercise, eat healthy. We all know right from wrong. And I don’t want to go into it, but I just want to say stop and think and be mindful and do what you’re supposed to do.
Number two, educating yourself with caution. I think it’s important. Look at the source you’re getting things from. Ask various people. Don’t just rely on one particular source. This is a time to educate yourself. This is a time to not panic. The source of information and using this time to take care of yourself mentally, physically and really, really help yourself and your loved ones and actually everybody get through this, this terrible thing we’re all experiencing.
Well, that is it for today. Don’t forget to subscribe for free, download and listen to Wellness Inc. with me, Dr. Mike Moreno on Apple Podcasts or wherever you listen. Follow me on social @The17DayDiet. Take care, guys. The Wellness, Inc. with Dr. Mike Moreno podcast is for informational and entertainment purposes only and is not intended as a replacement or substitution for any professional, medical, financial, legal, or other advice, diagnosis, or treatment. This podcast does not constitute the practice of medicine or any other professional service. The use of any information provided during this podcast is at the listeners own risk for medical or other advice appropriate to your specific situation, please consult a physician or other trained professional. Thank you.
About This Episode
On this episode of Wellness, Inc. Dr Mike Moreno interviews Dr. Raj Dasgupta host of the podcast “The Dr. Raj show” and quadruple certified in internal medicine, pulmonary, critical care and sleep.
Dr. Raj shares his experience treating patients on the front lines of Covid, the exciting new advances in COVID-19 care, and what you can do at home if your loved ones contract COVID-19.
The two discuss how people are dreaming differently and how people’s sleep has been impacted living through the pandemic.
Stay tuned for Dr. Mike’s weekly RX where he gives you his most helpful tips from this episode so you can take care of yourself and the people you love.
Connect with Dr. Raj Dasgupta
https://evergreenpodcasts.com/the-dr-raj-podcast
https://www.facebook.com/doctorrajd/
https://twitter.com/DoctorRajD
https://www.youtube.com/user/DoctorRajD/
https://www.doctorrajd.com/blog